“It’s just a PVD.”
GEORGE A. WILLIAMS, MD, OMIC Board of Directors
This issue of the OMIC Digest focuses upon the most common reason for a medical liability lawsuit: diagnostic errors and specifically diagnostic errors associated with retinal detachment. Detection of a retinal detachment or retinal pathology that may lead to a retinal detachment requires both an appropriate and timely clinical suspicion and the correct ocular examination.
Patients may present with a variety of complaints related to the primary mechanism of most retinal detachments, a posterior vitreous detachment (PVD). Flashes, floaters, spots, visual field loss manifesting as shadows or curtains, and simple loss of vision are the most common symptoms. The well-trained ophthalmologist typically recognizes such symptoms, but sometimes the message doesn’t get through. Perhaps there is a language problem, or in the course of a busy day the ophthalmologist fails to elicit or recognize the patient’s symptoms. Patients may fail to appreciate monocular symptoms or visual loss through denial or neglect. Unrecognized or unmentioned trauma may not be described for social or personal reasons. Regardless, it is our responsibility to determine the patient’s problem.
Once a diagnosis of retinal tear or retinal detachment is suspected, the ophthalmologist must proceed with an appropriate examination. The question of what constitutes an appropriate examination is often the focus of a medical liability claim. The American Academy of Ophthalmology Preferred Practice Pattern (PPP) on Posterior Vitreous Detachment, Retinal Breaks and Lattice Degeneration (available at aao.org) is an authoritative, peer-reviewed summary of the standard of care. All ophthalmologists who see such patients should be familiar with these recommendations. I can assure you that any plaintiff’s lawyer will be.
A couple of common issues repeatedly arise. The first is the need for a dilated examination with binocular indirect ophthalmoscopy and scleral depression. Some ophthalmologists (and many patients) are uncomfortable with scleral depression. However, the PPP clearly states that scleral depression is the standard of care whenever a retinal tear or retinal detachment is suspected. The second issue involves a suboptimal view due to media opacification such as cataract, vitreous hemorrhage, miosis, or poor patient cooperation. In such situations, B scan ultrasonography is required. If the ophthalmologist fails to perform either test, there is cause for concern.
 Fortunately, the vast majority of people (myself included) with symptoms consistent with a retinal tear or retinal detachment will have an uncomplicated PVD. However, even after an appropriate examination confirms the absence of a retinal tear or detachment, the treatment process is not over. The ophthalmologist must instruct the patient and, importantly, the office staff concerning the need to return as soon as possible if there is a change in symptoms or vision. An office protocol concerning how to address such phone calls or patient contacts is a good idea and an example is available at www.omic.com. It’s hard to do the right thing if you don’t see the patient at the right time.
Fortunately, the vast majority of people (myself included) with symptoms consistent with a retinal tear or retinal detachment will have an uncomplicated PVD. However, even after an appropriate examination confirms the absence of a retinal tear or detachment, the treatment process is not over. The ophthalmologist must instruct the patient and, importantly, the office staff concerning the need to return as soon as possible if there is a change in symptoms or vision. An office protocol concerning how to address such phone calls or patient contacts is a good idea and an example is available at www.omic.com. It’s hard to do the right thing if you don’t see the patient at the right time.
Diagnostic errors will always be inherent to the practice of medicine. That’s why you want a company with the financial strength and unsurpassed risk management programs of OMIC. The next time you think “It’s just a PVD,” remember one of Yogi Berra’s best aphorisms: “Never make the wrong mistake.”
OMIC declares another large dividend to be paid in 2018
We are pleased to announce a 20% dividend for policyholders renewing in 2018.
Since 2007, OMIC has declared dividends totaling more than $80 Million. To put this into perspective, on average, each of our physician policyholders has received cumulative credits equal to twice their annual premium. We are thrilled that our insureds have received two of the past ten years of coverage at essentially no cost – a tremendous return on the investment in our company. This good news is a direct result of our policyholder’s commitment to good medicine, which helps lower claim trends over time.
Our consistent return of premium places OMIC significantly ahead of our peer medical professional liability companies and is in line with a long-standing commitment to fiscal conservatism. From 2012 to 2016 alone, OMIC’s average yearly dividend of 20.8% far exceeded the average of 6.6% for other malpractice carriers. And, unlike many of our multispecialty competitors, we have returned all premium above what has been needed to prudently operate the company and maintain a strong surplus; and we’ve done so at the earliest opportunity.
The 2017 dividend will be payable as a 20% premium credit to insureds who renew their insurance with OMIC in 2018.
In addition, OMIC is also happy to announce that rates in all states and territories will remain unchanged throughout 2018. OMIC’s premiums in recent years remain quite competitive and we will do everything in our power to keep them as low as possible going forward.
We know that our success depends on our insureds continuing support of OMIC. Thank you for your loyalty and we hope you will spread the good news to colleagues who have not yet joined our company.
Diagnostic advice from the experts
ANNE M MENKE, RN, PhD, OMIC Patient Safety Manager
As reported in the lead article, our recent study of diagnostic error (DE) claims showed that the ophthalmologist’s care was the primary factor in the delayed diagnosis of retinal detachments (RDs). Experts evaluating such malpractice claims have the advantage of knowing the patient’s outcome and reviewing the records generated by all staff members and providers. They strive to understand the ophthalmologist’s decision-making process, and may support care they understand even if they would have handled the situation differently. They might ask the following questions to evaluate the care: How did the ophthalmologist decide which exams or tests to perform? What were the results? What determined whether to monitor a patient or refer to a retina specialist? What was the patient told? The reviews help identify breakdowns in the process of care. Here are some pearls extrapolated from these RD claims.
Q. The lead article noted that most patients in the study had RD risk factors. What caused ophthalmologists to miss them?
A. Experts reviewed the patient complaint and history provided to both practice staff members and the ophthalmologist to obtain a more complete assessment of risk factors. They noted many problems with obtaining, communicating, and documenting the presenting complaint and the history. At times, the staff member did not inform the ophthalmologist of reported symptoms or history (indicating both the need for education on RDs and a clear process for how to communicate this information). At other times, the ophthalmologist did not read the notes generated by the staff member that day, or his own notes from previous exams. It was especially difficult to defend an ophthalmologist when this key information was readily available in the medical record.
Q. When must I perform a dilated exam?
A. Experts largely based their opinion on the need for a dilated exam on the presence of risk factors for RD. Experts expected ophthalmologists to perform a dilated exam in patients with risk factors who reported a sudden vision loss or visual disturbance. For example, they felt fundus exams were required in patients with a history of lattice degeneration accompanied by a new complaint of floaters, those who complained of black spots after cataract surgery or reported recent eye trauma, before deciding that cataracts were the cause of the visual decline after trauma, and when there was no explanation for the vision loss. They often criticized ophthalmologists who did not perform dilated exams when longstanding patients with chronic eye conditions reported a recent, sudden decrease in vision.
Q. Do I have to perform scleral depression (SD)?
A. Experts had mixed opinions on the need for SD. They noted that comprehensive ophthalmologists (COs) do not always perform SD, even though the PPP from the AAO recommends it. They also acknowledged that patient complaints about discomfort often influence the decision to forgo SD. They were less critical of COs who did not perform SD if the patient was promptly referred to a retina specialist. In contrast, the experts felt that retina specialists should perform SD. They understood why an experienced retina surgeon who had a good view of the entire retina might not feel one was needed, but testified that they personally always perform one. All felt that documented SD would have significantly helped defend the care.
Q. What do I need to document?
 A. Experts opined that ophthalmologists should document when dilated exams are done, whether SD was performed (and if not, why not), and the results of confrontational visual fields. They should include drawings of the retina. Positive and negative findings are both important, so ophthalmologists should include pertinent findings, such as the absence of tears, RDs, lattice, or hemorrhage. Document education about RD warning signs, including the provision of written instructions or brochures, as well as telephone advice.
A. Experts opined that ophthalmologists should document when dilated exams are done, whether SD was performed (and if not, why not), and the results of confrontational visual fields. They should include drawings of the retina. Positive and negative findings are both important, so ophthalmologists should include pertinent findings, such as the absence of tears, RDs, lattice, or hemorrhage. Document education about RD warning signs, including the provision of written instructions or brochures, as well as telephone advice.
Q. When should I refer my patient to a retina specialist?
A. Comprehensive ophthalmologists should consider early referral to a retinal specialist if they do not have a clear view of the back of the eye (e.g., vitreous hemorrhage present). COs should refer patients with a history of trauma if no SD was performed or if a clear view of the retina out to the ora serrata cannot be obtained. COs who put RD lower on the differential should reconsider and refer patients when diagnostic studies refute the initial diagnosis, when the diagnosis does not correlate with the patient’s complaints, and when there is no explanation for the vision loss. COs should have an especially low threshold for referring any such patients if they have known risk factors for RD.
Failure to diagnose a RD by a comprehensive ophthalmologist
RYAN M BUCSI, OMIC Claims Manager
A 57-year-old corrections officer presented to an OMIC insured comprehensive ophthalmologist on referral from the emergency department. The patient reported a fall at work where he struck the left side of his head, face, and hip. He explained that his vision became blurred after the fall. His vision was 20/40 OU with bilateral cataracts. The IOP OS was 9, which was low compared to the IOP OD. The insured referred the patient back to his primary care physician. One month later, the patient returned to the insured’s office and the insured noted a decrease in visual acuity to 20/125 OS; the IOP was still 9. The insured attributed the worsening vision to progressive cataracts OS>OD and referred the patient to a colleague for surgery, which was performed two months later. On postoperative day 3, the patient’s vision had further decreased to 20/150 OS. The insured diagnosed a retinal detachment and emergently referred the patient to a retina specialist. The following day, the retinal specialist performed a pars plana vitrectomy with laser to reattach the retina. Subsequently, the patient had two recurrent retinal detachments with scar tissue requiring two additional surgeries, a gas bubble injection and the placement of silicone oil. The retina specialist noted that any return of vision OS was unlikely. The patient’s final visual acuity was HM.
Analysis
 Plaintiff expert’s theory was that the patient suffered a traumatic tear of a portion of his retina OS as a result of the fall and that the initial OMIC insured failed to diagnose this detachment despite it becoming progressively more severe during the time he saw the patient. As a result of this delay in diagnosis, the ability to re-attach the retina, once the detachment was diagnosed, was significantly lessened and was a substantial factor in bringing about the permanent loss of sight OS. The plaintiff experts were critical of the first OMIC insured since the patient associated the blurry vision OS with the fall from the moment it happened; the discrepancy in IOP between the right and left eyes with the left eye pressure being much lower after the fall than for the many years preceding it; the worsening visual acuity during the first month after the traumatic incident as further evidence of continued retinal detachment; and a rather superficial initial examination and lack of a dilated and funduscopic examination. Unfortunately, our defense experts agreed with plaintiff expert’s opinions on this case. Our experts believed that the second insured (the cataract surgeon) could also potentially be criticized for not performing a dilated examination prior to the performance of the cataract surgery. The plaintiff’s case was strengthened when the retina specialist testified at his deposition that the patient suffered a traumatically induced retinal detachment as a result of the fall. The retina surgeon declared that the detachment progressively worsened over the next few months. Due to the retina specialist’s impartial position in the case and his firm statements, he became the best expert for the plaintiff. Defense counsel estimated the likelihood of a plaintiff verdict at 80%. As a result, mediation was scheduled and the case settled for $475,000 on behalf of the fist insured, as he essentially took the blame for the substandard care, thus prompting plaintiff to dismiss the second insured and the group.
Plaintiff expert’s theory was that the patient suffered a traumatic tear of a portion of his retina OS as a result of the fall and that the initial OMIC insured failed to diagnose this detachment despite it becoming progressively more severe during the time he saw the patient. As a result of this delay in diagnosis, the ability to re-attach the retina, once the detachment was diagnosed, was significantly lessened and was a substantial factor in bringing about the permanent loss of sight OS. The plaintiff experts were critical of the first OMIC insured since the patient associated the blurry vision OS with the fall from the moment it happened; the discrepancy in IOP between the right and left eyes with the left eye pressure being much lower after the fall than for the many years preceding it; the worsening visual acuity during the first month after the traumatic incident as further evidence of continued retinal detachment; and a rather superficial initial examination and lack of a dilated and funduscopic examination. Unfortunately, our defense experts agreed with plaintiff expert’s opinions on this case. Our experts believed that the second insured (the cataract surgeon) could also potentially be criticized for not performing a dilated examination prior to the performance of the cataract surgery. The plaintiff’s case was strengthened when the retina specialist testified at his deposition that the patient suffered a traumatically induced retinal detachment as a result of the fall. The retina surgeon declared that the detachment progressively worsened over the next few months. Due to the retina specialist’s impartial position in the case and his firm statements, he became the best expert for the plaintiff. Defense counsel estimated the likelihood of a plaintiff verdict at 80%. As a result, mediation was scheduled and the case settled for $475,000 on behalf of the fist insured, as he essentially took the blame for the substandard care, thus prompting plaintiff to dismiss the second insured and the group.
Risk management principles
The first insured performed only a cursory examination. He did not appear to take the recent fall into account when evaluating the vision loss. The diagnosis of cataracts could potentially explain the blurry vision, but the reason for the asymmetrical lower IOP was not explored. According to all experts in this case, the sudden vision loss and asymmetrical IOPS should have set off alarm bells. However, the insured did not appreciate or explore other explanations for the visual complaints once he diagnosed bilateral cataracts. Furthermore, the insured did not perform a dilated examination, which was indicated based on the patient’s presenting complaints and recent history of trauma. Had this been done it is more than likely that the insured would have discovered a retinal detachment, which would have increased the odds of all or some vision being saved OS. In addition, the lack of a dilated exam prior to cataract surgery represents another missed opportunity to have diagnosed the retinal detachment.
Failure to diagnose retinal detachments
 ANNE M MENKE, RN, PhD, OMIC Patient Safety Manager
ANNE M MENKE, RN, PhD, OMIC Patient Safety Manager
In a recent study of OMIC diagnostic error (DE) claims, we learned that those involving a retinal condition were the most common, accounting for 38% of the claims closed between 2008 and 2014. By far, the most frequently missed diagnosis in our entire study was retinal detachment (RD). The RD claims represent 79% of the DE retina claims and 48% of the DE retina payments. Remarkably, while there were only six claims for failure to diagnose retinopathy of prematurity, those claims comprised 47% of the DE retina payments.
This issue of the Digest will explore RD DE claims in more detail, first by
presenting data and analysis and then by offering recommendations. The management of RDs once they were diagnosed did not affect the outcome of these claims, so our analysis will focus solely on the diagnostic process.
Forty-two claimants in the study alleged a delay in the diagnosis of RD during the noted 7-year period. They ranged in age from 20 to 79 years of age, with the majority in their 50s and 60s. The delay period ranged from one week (or less) to 32 weeks (Figure 1).
There was no clear relationship between the alleged delay period and indemnity payments. When the diagnosis closely followed the ophthalmologist’s examination, however, claimants had an easier time arguing that the RD was present but missed. Claimants had more difficulty proving negligence when there was a long period between the exam and the eventual diagnosis, although other factors sometimes led to a decision to settle the claim. Visual acuity deteriorated significantly during the alleged delay period, as shown in Figure 2.
The number of claimants with good vision (≥ 20/40) declined from 25 at the initial encounter to 9 at the final encounter, while those with poor vision (<20/200 to LP) doubled; two claimants who had light perception at the initial encounter ended up with no light perception.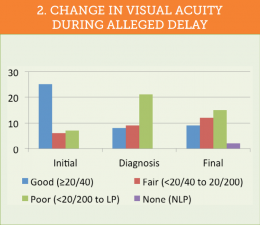
Analysis of OMIC defendants and indemnity payments
The number and type of OMIC-insured defendants in the RD DE claims varied. Twenty-five claims were filed against a sole defendant (22 against a single ophthalmologist, 3 against a group); the other 17 claimants named multiple defendants, for a total of 63 claims. Although 40% of the claims involved multiple defendants, OMIC never paid on behalf of more than one defendant. Multiple defendants did increase the costs of defending the care, however.
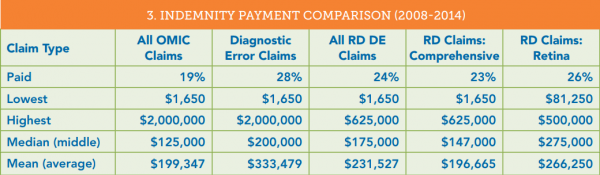
DE claims are costly. When compared to all OMIC claims during the study period, claims alleging DE of any type resulted in more paid claims, a higher median and mean payment, and the highest payment. DE claims alleging failure to diagnose RD had a slightly lower percentage of paid claims than overall DE claims, as well as lower median, mean, and high payments. Nonetheless, RD claims still had higher median and mean payments than other OMIC claims as a whole (see Figure 3). Comprehensive ophthalmologists (COs) provided the care in 70% of the RD claims, retina specialists (RSs) in the remaining 30%. OMIC made indemnity payments on behalf of a higher percentage of RSs than COs, and the payments tended to be for larger amounts. The small number of claims and payments makes it hard to draw firm conclusions, but experts may have held RSs to a higher standard than COs. The lowest DE payment of $1650 was made on behalf of a CO to reimburse the claimant in an RD claim for out-of-pocket expenses. The highest overall DE claim was for an oncology condition. The highest RD DE payment, for both COs and RDs, was made to a surgeon whose loss of binocular vision affected the ability to perform surgery.
Initial diagnosis and risk for RD
Two of the forty-two RD DE claimants in the study received only telephone care. Ophthalmologists diagnosed 21 of the remaining 40 claimants with a retinal condition other than RD. Retinal conditions diagnosed at the initial encounter in descending order of frequency were posterior vitreous detachment (PVD); vitreous changes such as floaters, degeneration, or syneresis; retinal tear; traumatic injury other than PVD or tear; endophthalmitis following cataract surgery; and non-proliferative diabetic retinopathy with lattice degeneration. The other 19 initial diagnoses, in descending order of frequency, were refractive errors including cataract; neurological conditions; postoperative changes following cataract surgery; glaucoma; and medical conditions (GCA and collagen vascular disease).
The AAO’s Preferred Practice Pattern “Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration” states that risk factors for developing an RD are retinal breaks, myopia, lattice degeneration, cataract surgery, trauma, and a history of RD in the fellow eye or in the patient’s family. As Figure 4 shows, 34 of the 39 claimants (85%) who were given a diagnosis other than RD had one or more of these risk factors at the time of the initial visit. Did the defendant ophthalmologists lack knowledge of the relationship between these conditions and RD? Did they neglect to obtain a history and perform an exam likely to uncover an RD? Did they fail to educate the claimants with risk factors about the condition and the symptoms that should be reported to the ophthalmologist? Did claimants not recognize the symptoms or neglect to notify the ophthalmologist? Experts for both the claimants and defendants sought answers to these questions when they conducted their reviews.
Standard of care (SOC) and causation analysis
As expected, claimant experts concluded that at least some aspect of the care was negligent in the RD DE claims in this study. What did defense experts decide? They reviewed 54 of the 63 claims (9 closed without payment before a review was completed). Additional reviews were usually obtained if the initial one raised concerns. If the reviewers reached different conclusions, we considered this a “mixed” review. According to these experts, the defendant met the standard of care 56% of the time, and failed to do so in 44% of cases (Figure 5). One would expect comprehensive ophthalmologists to have more difficulty diagnosing RDs than retina specialists, and they did: comprehensive ophthalmologists had negative reviews 50% of the time, while defense experts criticized the care of retinal specialists in 29% of the cases.
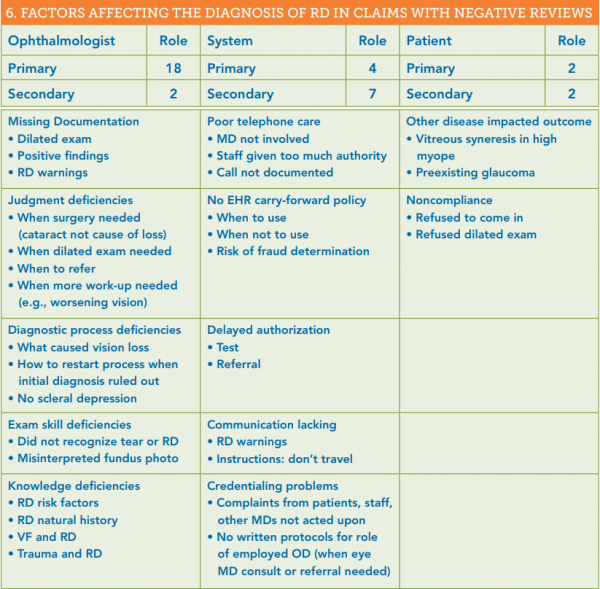
This condition clearly presents diagnostic challenges to many ophthalmologists. Why is that? To help answer that question, we evaluated claims with negative reviews for the role ophthalmologists, systems (scheduling, telephone care, etc.), and patients played in the delay. All claims had primary causes, while only some had secondary causes. As Figure 6 shows, physician factors account for twice as many delays as systems issues, while patients had the least impact. Specific examples of areas of concern in each category are shown.

Moving from examination to education to diagnosis
As Figure 4 showed, 85% of the patients had risk factors for RD at the time of the initial diagnosis. What obstacles stand in the way of an earlier diagnosis of an RD? The short answer is teamwork. First, the ophthalmologist needs to obtain an adequate history and recognize the risk factors. The Hotline article in this issue provides more detail on what defense experts found lacking in the ophthalmologist’s care. Next, the physician and staff members need to educate the patient about the symptoms and the process for reporting them. Staff members who answer phones need to have written protocols on how to schedule appointments, and have knowledge of symptoms that require urgent or emergent appointments.
The goal of patient education about RDs is to elicit the patient’s agreement to monitor for and report worrisome symptoms. Patient engagement will not happen if the patient does not understand the information, is too distracted by fear of vision loss, or hears only the reassuring news that no RD was found that day. Patients may be confused about the uncertainty and not be able to understand that they may never develop an RD, have one within days, or not for many months. The time gap between the education and the appearance of symptoms can be quite long. The patient can forget the information or lose the written instructions. If the gap is short and the symptoms are the same as the first visit, the patient may decide that there is no need to call, or that she does not have the funds to return so quickly for another visit. Staff who seem brusque or unwelcoming, or lack the knowledge to understand the significance of the reported symptoms, could lead patients to stop advocating for themselves and put off a return visit.
Prompt diagnosis of an RD requires an informed, engaged, and welcoming team. Use an RD risk factor and symptom checklist to train staff on how to help identify patients at risk. Include staff in the development of written protocols for telephone care. Ask them to let you know if they feel the patient doesn’t understand or hasn’t committed to monitoring. Give patients specific language to use to signal a possible RD when they call, such as “Dr. Williams said to bring me in right away if I had this symptom.” In addition, sound like you mean it when you invite patients to call you.
1. See the Digest issue on diagnostic error at https://www.omic.com/diagnostic-error-types-and-causes/.






