Message from the Chair

Tamara Fountain MD, OMIC Chair
I spent this past Mother’s Day at my grandmother’s house in Appalachian Virginia.
Granny is 89 years old and still lives independently in the house my grandfather built almost 50 years ago. She remains witty, often ribald, and cognitively sharp as a tack, but each time I return to her Blue Ridge Mountain hamlet, I notice small, but real and progressive changes in her motor abilities. She fell out of the blue in a bank parking lot several months ago. While nothing was broken, the experience shook her confidence and was a sobering reminder to our extended family of the encroaching threats to her physical and emotional independence.
As you will read in this issue of the Digest, falls have a crippling impact on the quality of life in the elderly population. We ophthalmologists are second only to geriatricians in the percentage of elderly patients we see in our practices. Add to that the visual difficulties inherent to our patient population and you have the perfect recipe for an accident—and lawsuit—waiting to happen.
It’s not just the elderly we have to worry about either. As a plastics specialist, I am commonly probing, poking, cutting, and cauterizing patients in my office procedure room. I encounter a handful of vasovagal events in a year, usually in someone under 40. Swooning doesn’t necessarily have to occur in a visibly nervous patient or even during the procedure. A 20-year-old male patient in our practice had an uneventful chalazion incision and was conversant and calm throughout the procedure. He checked out at our front desk and took the elevator to the ground floor. Only when walking to his car, did he pass out, pitching forward onto his face and breaking his jaw, nose, and several teeth. This prompted my office to establish a protocol in which all patients undergoing even the most minor procedures are advised to bring a companion, not only to drive them home, but to escort them to their vehicle and home after the office procedure.
We see patients who are old, frail, and can’t see. We do office procedures that can trigger the fight or flight response in even the most stoic patient. Falls cause life-threatening injuries and can signal the beginning of the end in an elderly person’s life. The bigger they are, the harder they fall, so it is said. Anyone who has ever seen (or worse, heard) a human fall to the ground knows it is a hard and traumatic landing no matter the body type or age.
Falls by their nature are unexpected but we can do a better job of anticipating these events. By putting certain policies and procedures in place, you can protect your patients from bodily harm and you and your practice from litigation harm.
TAMARA R. FOUNTAIN, MD, OMIC Board of Directors
Insurance for tangential perils of medical practice
NAS Insurance Services has been chosen by OMIC as a preferred referral market for a range of business-related insurance products. Founded in 1975, NAS was the first to conceive of insuring businesses for legal expenses related to numerous perils they experience—a type of coverage not provided by typical liability insurance at the time.
The NAS Insurance Agency can help you shop for a variety of business coverages that are tailored specifically for ophthalmic practice. NAS accesses top-rated carriers and markets not available on a direct basis, including Lloyds of London. The agency can obtain competitive quotes for business owners policies and general liability coverage through major carriers such as The Hartford. As highlighted in this Digest, it is important to have appropriate and comprehensive coverage in place for slips and falls and other tangential perils of medical practice.
OMIC policyholders already have 14 insurance benefits provided under their standard malpractice policy that cover regulatory, fraud abuse, HIPAA, and eMD (cyber liability) exposures. Learn about the coverage you already have as an insured by visiting www.omic.com/policyholder/benefits.
To buy additional coverage for the regulatory and cyber benefits included in your malpractice policy or to learn about or purchase other common insurance products, such as business owners and workers compensation policies; employment practices, directors and officers, and managed care errors and omissions liability insurance; and ERISA fiduciary bonds, contact Dana Carulli at NAS at 877.808.6277 or dcarulli@nasinsurance.com.
Reduce exposures that can lead to patient slips and falls
There are some proactive steps you can take to make your office safer for patients.
- Make sure work areas are neat, clean, and orderly. Provide safe and adequate space for patients to maneuver around your office and exam rooms.
- Ensure that carpets and rugs are well secured to the floor to prevent bunching up or tripping hazards.
- Inspect outside areas. Redirect sprinklers aimed at pedestrian walkways and eliminate algae or mold that may have formed on surfaces, making them slippery. Correct uneven areas, cracks, or depressions in sidewalks or entrance areas.
Hip fracture in 90-year-old female patient following fall in exam room
RYAN BUCSI, OMIC Senior Litigation Analyst
Allegation
Failure to monitor/assist an elderly patient resulting in a fall.
Disposition
Settled for $100,000. OMIC’s contribution was $50,000.
Following a dilated eye exam, a 90-year-old patient began to get up from the examination chair. In the process, she scuffed her shoe on the floor, which caused her to twist and fall to the ground. An ophthalmic technician was in the room and was able to catch the patient’s upper body protecting her head from injury. When the OMIC-insured ophthalmologist reentered the room the patient stated that she had “lost her balance or something” and complained of right hip pain. Minimal assistance was required to help her into a wheelchair and she was taken to her automobile, which was driven by her daughter. The patient did not want emergency medical attention so she was advised to use Tylenol for pain and to call her family doctor should discomfort persist. The following day the patient was taken via ambulance to the emergency room for right hip pain. An orthopedic surgeon diagnosed a nondisplaced subcapital right hip fracture and noted that the left hip had screws that were placed after a prior fracture. Moderate to advanced degenerative joint disease was also diagnosed in both hips. The fracture required surgery during which three cannulated screws were placed under fluoroscopic guidance. The patient was discharged from the hospital to a convalescent home, where she spent 45 days. She was then discharged to her home with progressive weight bearing allowed. At her last visit with the orthopedist, she described occasional right hip pain. Passive range of motion caused no discomfort.
Analysis
OMIC’s defense counsel retained an orthopedic expert who opined that the patient experienced a spontaneous or indirect traumatic subcapital hip fracture that caused her to fall. She had suffered a broken left hip approximately one year prior to this incident when she fell while boarding a bus. The bus driver caught her, but she still fractured her left hip. In our expert’s opinion, no matter how attentive the technician was, she would not have been able to prevent the fall and in fact did a good job of breaking the fall enough to prevent a serious cranial injury. The patient testified at her deposition that she was blind and could not see as a result of the dilated exam. She claimed that she called out to the ophthalmic technician for assistance, but the technician did not respond so she decided to get up on her own. The issue in this matter was whether the ophthalmic technician had a duty to escort the patient to the lobby and out of the building, and if so, whether she was negligent in performing this duty. Plaintiff counsel brought two claims in this case. The first was a medical negligence claim against the OMIC-insured ophthalmologist and the second was a general negligence claim against the OMIC-insured entity that employed the technician. Therefore, OMIC and the premises liability carrier jointly represented the entity. Unfortunately, the county in which this fall occurred was known to be a plaintiff-friendly venue. Although our defense counsel was confident about our chances for a defense verdict, he did advise that a plaintiff verdict could result in a $250,000 to $400,000 award. This case was therefore taken to mediation where a settlement of $100,000 was negotiated. OMIC and the premises liability carrier agreed to spilt the settlement 50/50. The settlement was negotiated on behalf of the entity since the ophthalmologist was not even in the room at the time of the fall. The OMIC insured was dismissed from the lawsuit and no report to the National Practitioner Data Bank or state medical board was required.
Risk management principles
During the claims investigation, it became clear that this particular patient had many risk factors for a fall. She was 90 years old and had fallen and broken her left hip the previous year. She also had just had her eyes dilated during an ophthalmic examination. The Hotline article provides a quick screening tool of questions that help determine who might need assistance. Knowing about this patient’s recent fall and hip fracture would have alerted the technician to stay with the patient and assist her in standing up and walking back to the lobby where relatives or other caregivers could take over assisting her back to the car.
Help patients reduce their risk of falling in your office or ASC
ANNE M. MENKE, RN, PhD, OMIC Risk Manager
In response to the high number of older patients injured in falls each year, the Centers for Disease Control (CDC) developed a program called STEADI: Stopping Elderly Accidents, Deaths, and Injuries. Many of the materials are geared to primary care physicians and include strength, balance, and mobility tests. Ophthalmologists in their offices and staff in ambulatory surgery centers (ASCs) are not likely to perform these tests as part of an eye exam or preoperative evaluation. The information in the documents does, however, contain recommendations that can be implemented by the eye care team.
Q We have a busy practice and see many elderly patients. Is there a real-world tool our staff members can use to determine who is at risk of falling?
A Yes. One simple way to screen for fall risk is to ask the patient three questions proposed by the CDC: (1) Have you fallen in the last year? (2) Do you feel unsteady when you stand up or walk? and (3) Do you worry about falling? Some ASCs skip the CDC’s third question about the fear of falling and instead ask if the patient has a history of dizziness or lightheadedness, which can help identify younger patients who suffer vasovagal episodes in medical settings. Staff can either ask the questions and document the answers or include them on forms the patient completes, such as the one identifying who will drive them home after surgery or their emergency contact information. Any yes answer indicates the need for assistance and should be communicated to all members of the team providing care for the patient.
Q What are the signs of gait or balance problems?
A Certain behaviors that are readily observed can point to unsteadiness and increased fall risk. Ask staff to watch for these behaviors and immediately go to the side of any patient who exhibits them. Using one’s hands to push up off a chair, a sign of weak abdominal or leg muscles, could alert staff to stand next to the patient and provide assistance. Holding onto furniture when walking could indicate a fear of falling or weakness in the extremities. Trouble stepping up to a curb could stem from poor depth perception or muscular problems. Many patients experience urinary urgency and may fall while rushing to the bathroom. Offer these patients assistance to the restroom, especially after sedation or anesthesia. Patients who use mobility aids, such as canes, walkers, and wheelchairs, are easy to notice. It can be hard to know when to help, however. Our claims experience shows that some may value their independence and decline offers of assistance. Respect the patient’s choice but stay with the patient and be prepared to help until she has safely moved to where she is going. It might be surprising to learn that patients who are sad or depressed are at increased risk of falling. Perhaps they are less attentive to their environment and don’t notice obstacles or the approach of steps as readily. Will getting answers to these questions and observing these behaviors prevent falls in ophthalmic practices and surgery centers? From the limited information available in the claims files we analyzed of 41 patients who fell, at least 19 of the patients would have been considered at increased risk for a fall based on their histories or behaviors. Asking the patient if he or she worries about falls or feels unsteady or lightheaded could well have identified more.
Q Are we expected to educate patients about their increased fall risk?
A Just as ophthalmologists and ophthalmic ASCs do not conduct formal gait and balance testing, they are not expected to provide extensive education on fall risk. But the eye care team can advise patients of simple ways to keep themselves safe. Consider placing signs with the following reminders in the lobby or examination lanes. Prevent falls that can occur when standing up from a seated position by suggesting: “stand up slowly” and “stand still a minute after you stand up.” When patients are offered sunglasses and prepare to exit into brighter light, remind them to “take your time” and “wait for your eyes to adjust.”
Q Our office does not have equipment to lift or move heavy patients. We are worried that staff may injure themselves by trying to assist bigger patients.
A These fears are well-founded. The CDC website’s section on workplace safety indicates that the healthcare industry has some of the highest reports of musculoskeletal injuries from what it calls “overexertion.” The single greatest risk factor for overexertion injuries is the manual lifting, moving, and repositioning of patients. According to the CDC, mechanical equipment, not staff, should be used to lift and move patients: there is no safe way to manually lift another adult human being. Let the ophthalmologist or head nurse know if you identify a patient who needs lifting or moving. The patient may need to be sent to a facility with the necessary equipment.
When patients fall, are doctors to blame?
ANNE M. MENKE, RN, PhD, OMIC Risk Manager
Mrs. B, a 73-year-old woman with a number of medical conditions, came to her ophthalmologist’s office for an eye exam. She was asked to sit on a stool with wheels for the exam. She slipped off, landing on her tailbone. X-rays revealed a possible hairline fracture of the spine. When Mrs. B suffered bruising and ongoing pain, she filed a claim against the ophthalmologist. She never regained the ability to walk and died nine months later. Her claim settled for $60,000.
Falls are the leading cause of fatal and non-fatal injuries for people over 65 years of age, according to the Centers for Disease Control (CDC). They stem from intrinsic factors related to the individual, such as age, health problems, and medications. Or they can result from extrinsic, environmental circumstances, such as wet floors or poor lighting. A fall compounds the burden of preexisting health problems and can precipitate an inexorable decline. Indeed, 20% of older people who fall die within one year of the mishap, like the patient discussed above. Many of these falls occur in the home. When they happen in physician offices and ambulatory surgery centers (ASCs), some patients and their families assume that physicians and staff members should have predicted and prevented the fall, and they sue for malpractice.
OMIC has handled 50 claims and lawsuits involving 41 patients who have been injured during falls, about 1% of our total claims since 1987. Of these 50 claims, 46 are now closed. The 41 patients who filed these claims are similar to those studied by the CDC: all but ten were over age 60, and four died, three within the first year after the accident. Forty patients sustained significant injuries and faced unexpected medical costs. Twenty-five had fractures, including of the skull, nose, arms, ribs, spine, hip, legs, and feet. The remaining patients had rotator cuff tears or serious soft tissue injuries to the head, hip, and upper and lower extremities. But were the falls due to negligent care? Could they have been prevented? This issue of the Digest will examine the circumstances surrounding falls, determine factors that increase their likelihood, and offer suggestions on ways to identify and assist those most at risk.
When is a fall the result of negligent care?
When patients who fall sue their ophthalmologists, they usually allege that the fall should have been prevented by maintaining a safer environment, better assisting the patient, or both. Therefore, most investigations of fall claims will include not only an analysis of the patient’s medical condition and the care provided by the ophthalmologist and staff, but also a review of the environment.
Such an investigation was conducted after a 79-year-old woman who presented for a dilated eye exam fell and sued her ophthalmologist. As they had done after all of her prior dilated exams, the ophthalmologist’s staff members offered her sunglasses as she was leaving the office to help reduce her light sensitivity. She declined the offer. After she exited the darker office into the sunlight, she lost her balance on a set of stairs and fell down, breaking her hip. An analysis of the incident showed that the patient was healthy and the care of the ophthalmologist’s staff was appropriate. The attorney defending the physician then conducted an inspection of the premises. He noted that the first step was about eight feet from the door. There were handrails on both sides and down the middle of the stairs. Each step was three feet long, with the edge painted black. He felt that the steps were constructed as safely as possible and were in good condition. He concluded that even if the patient was temporarily “blinded” by the bright sunlight as she claimed, she nevertheless had space and time to allow her eyes to adjust before starting down the stairs. The attorney filed a motion for a summary defense judgment as no expert had alleged that the eye physician or his staff had been negligent, perhaps because this was a healthy patient who knew what to expect after dilation and declined the offer of sunglasses. The motion was granted, and the case was dismissed.
In fall-related lawsuits, plaintiffs may allege professional liability (PL or medical malpractice) or general negligence (GL or premises liability). Professional liability is negligence based on a breach of the standard of care in the performance of healthcare services. Premises liability occurs when a business owner does not adequately protect its patrons from hazards on the premises. Therefore, in order to determine whether a case is really a PL or GL claim, courts will often look at whether the patient was actually receiving medical care at the time of injury. They may also look at whether the service being provided requires special knowledge, licensing, or accreditation. This distinction is important for a variety of reasons that are explained in the Policy Issues article.
Payments for falls
The decision to settle a claim is usually based upon reviews provided by OMIC’s consultants or experts hired by the defense attorney, and after consultation with and consent from the insured ophthalmologist or ASC. However, it is not always necessary to obtain expert opinions for claims when patients fall, as the injuries are evident and the allegations and investigations relatively straightforward. OMIC settled 18 of the 46 closed claims (39% of them) related to falls. This percentage is almost twice as high as for our claims experience overall (see table 1). There are several reasons for this. 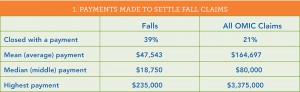
First, ophthalmologists, their practices, and ophthalmic ambulatory surgery centers often quickly elected to settle claims involving severe injuries, obviously frail patients, or those using assistive devices, such as canes, walkers, or wheelchairs.
Second, while physicians were often named as defendants in these claims, the falls generally occurred while the patient was with staff. Accordingly, settlements were made on behalf of the practice or ASC and the physician was dismissed from the claim. Such a resolution has an added benefit: while indemnity payments made on behalf of physicians and other licensed healthcare practitioners must be reported to the National Practitioner Data Bank, no such report is required for entities.
Finally, the mean and median payments were significantly less than for OMIC’s total claims, as was the largest payment. The highest payment for a fall occurred after an 82-year-old woman fell when asked to move onto a chair with wheels. When the chair went out from under her, she fractured her hip. She required surgery, an extensive hospitalization, and care in a nursing home, leading to $100,000 in medical expenses. When Medicare learned how the fracture occurred, it refused to pay for her care. OMIC settled the claim for $235,000. (OMIC’s highest-ever indemnity payment of $3,375,000 was for failure to diagnose retinopathy of prematurity.)
When and where do eye patients fall?
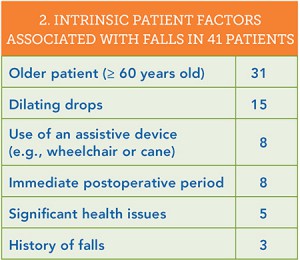 In an attempt to learn what can lead to falls, we analyzed both the patient characteristics associated with the falls and the actions that immediately preceded them (see tables 2 and 3). Thirty of the 41 patients fell during or just after office visits; the remaining 11 fell at an ambulator
In an attempt to learn what can lead to falls, we analyzed both the patient characteristics associated with the falls and the actions that immediately preceded them (see tables 2 and 3). Thirty of the 41 patients fell during or just after office visits; the remaining 11 fell at an ambulator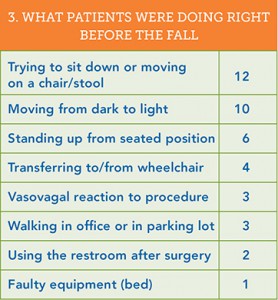 y surgery center. After the patient’s age, the most common intrinsic factor associated with a fall was the use of dilating drops: fully half of the patients who fell at the office did so after a dilated eye exam. Dilating drops are an essential aid to diagnosis. Yet they are known to cause temporary vision problems, such as light sensitivity, glare, and decreased contrast sensitivity. These drops may be more apt to pose problems for older patients since it can take longer for their eyes to judge distance and depth and to adjust to sudden changes from dark to light. Indeed, 10 patients fell when moving from the darker interior of the office into the brighter outdoors, including patients wearing sunglasses or transitional lenses.
y surgery center. After the patient’s age, the most common intrinsic factor associated with a fall was the use of dilating drops: fully half of the patients who fell at the office did so after a dilated eye exam. Dilating drops are an essential aid to diagnosis. Yet they are known to cause temporary vision problems, such as light sensitivity, glare, and decreased contrast sensitivity. These drops may be more apt to pose problems for older patients since it can take longer for their eyes to judge distance and depth and to adjust to sudden changes from dark to light. Indeed, 10 patients fell when moving from the darker interior of the office into the brighter outdoors, including patients wearing sunglasses or transitional lenses.
The most frequent action leading to a fall was moving onto a chair or stool or changing position while on one. Experts who reviewed claims involving falls from stools or chairs with wheels criticized their use, especially in elderly patients who were left unattended. Standing up from a seated position precipitated six falls. Older patients may experience drops in blood pressure when standing up and thus feel faint. This is even more likely right after surgery involving sedation or anesthesia: eight patients fell in the immediate postoperative period. Older patients often do not have strong muscles in their abdomen or legs and need to use their hands to push off from chairs to stand up. Younger ones who fell when getting up had vasovagal episodes after injection of fluorescein or minor eye procedures. Eight patients fell who used mobility aids, such as canes, walkers, and crutches, including four patients who fell while moving into or out of their wheelchairs.
What assistance should be offered to patients?
This review of 41 falls offers some guidance on which patients are likely to fall, and the Hotline article provides additional screening tools. By asking some simple questions and watching for certain behaviors, ophthalmologists and the eye care team can identify those most at risk. The next step in fall prevention is to provide assistance. But which patients should be helped? Are staff in offices expected to escort each patient whose eyes have been dilated to the front desk? Should they and staff at ASCs take all patients to their cars? Eye practices and ASCs clearly do not have the personnel to provide this level of individual assistance. And while plaintiff attorneys have alleged that this help was required and should have been provided, experts hired by defense attorneys to evaluate fall claims did not agree. They made it clear that staff should not be expected to assist patients who function normally outside the office, even if their eyes are dilated. They were critical, however, when the physician and staff did not provide monitoring and assistance for patients who had obvious difficulty ambulating and moving.
Back in 1992, OMIC Board member Dr. Monica L. Monica offered some “common sense safety tips” to minimize the likelihood of a general liability claim (http://www.omic.com/making-your-office-safe/). Her suggestions on which patients to assist are still pertinent today. Please see her article for more detailed advice on making the office environment safe.
- Watch and assist patients when seating them on stools. Make sure the rollers of the stool do not easily slide, carrying the stool out from under the patient. Stools with locking devices are preferable, especially when performing office laser procedures.
- Supervise and assist patients with mobility problems at all times when being moved in and out of exam rooms or on and off chairs. This is especially important for individuals who are blind or have low vision.
- Stay with elderly patients in exam or treatment rooms.
- Encourage patients whose pupils have been dilated to stay in the office until they are comfortable with their vision. Provide post-mydriatic spectacles or drops to reverse dilation. Suggest that patients take a taxi home or arrange for a family member or friend to drive them.
Falls cause significant injury. Ophthalmologists and the entire eye care team can help prevent them. To assist in staff education, key information in this issue of the Digest has been summarized in “Fall Prevention,” available at http://www.omic.com/fall-prevention/.







